Updated April 26, 2020, 10 p.m. PT. The following sections have been updated or added in the past 48 hours: Ophthalmology ties
The Academy is sharing important ophthalmology-specific information related to the novel coronavirus, referred to as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The highly contagious virus can cause a severe respiratory disease known as COVID-19.
This page is principally authored by James Chodosh, MD, MPH, with assistance from Gary N. Holland, MD, and Steven Yeh, MD.
What you need to know
- Several reports suggest that SARS-CoV-2 can cause a mild follicular conjunctivitis otherwise indistinguishable from other viral causes, and possibly be transmitted by aerosol contact with conjunctiva. However, at this point in the COVID-19 pandemic, practically any patient seen by an ophthalmologist could be infected with SARS-CoV-2, regardless of presenting diagnosis, risk factors, indication for visit or geographic location.
- SARS-CoV-2 is susceptible to the same alcohol- and bleach-based disinfectants that ophthalmologists commonly use to disinfect ophthalmic instruments and office furniture. To prevent SARS-CoV-2 transmission, the same disinfection practices already used to prevent office-based spread of other viral pathogens are recommended before and after every patient encounter.
- The Academy and federal officials strongly recommend protection for the mouth, nose and eyes when caring for patients potentially infected with SARS-CoV-2.
Background
SARS-CoV-2 is an enveloped, single-stranded RNA virus that causes COVID-19. It is highly transmissible and has a significant fatality rate, especially in the elderly and those with comorbidities such as immune suppression, respiratory disease and diabetes mellitus. A significant number of global fatalities have occurred, and the impact is being felt worldwide.
Patients typically present with respiratory illness, including fever, cough and shortness of breath; diarrhea is common early in infection, and conjunctivitis has also been reported. Other less specific symptoms include headache, eye pain and fatigue. Complications in severe cases include pneumonia, renal failure, cardiomyopathy, stroke and encephalopathy. Symptoms can appear as soon as 2 days or as long as 14 days after exposure. A March 10 study in the Annals of Internal Medicine found that the mean incubation period for SARS-CoV-2 was 5 to 7 days, and patients were typically infectious for several days prior to symptom onset. More than 97% of those who developed symptoms did so within 11.5 days of exposure, findings that further support current 14-day quarantine recommendations.
Transmission
Current understanding about how COVID-19 spreads is based largely on what is known about other similar coronaviruses. The virus is believed to spread primarily via person-to-person through respiratory droplets produced when an infected person coughs or sneezes. It also could be spread if people touch an object or surface with virus present from an infected person, and then touch their mouth, nose or eyes. Viral RNA has also been found in stool samples from infected patients, raising the possibility of transmission through the fecal/oral route.
Existing evidence suggests that SARS-CoV-2 is commonly spread by asymptomatic and presymptomatic transmission. A Feb. 21 report in JAMA details a case of an asymptomatic carrier who possibly infected 5 family members despite having normal chest computed tomography (CT) findings. In an outbreak at a long-term care skilled nursing facility in King County, Washington, 30% of residents tested positive for SARS-CoV-2; half of these were asymptomatic on the day of testing. In another study from China, the transmission rate from those with “undocumented” infections (asymptomatic or symptomatic but not meeting testing criteria) was lower but still significant, with an estimated transmission rate about half that of those with classical symptoms. Because undocumented infections are more common than current testing levels can account for, they may serve as a greater source of transmission than those of symptomatic carriers who have tested positive. The median duration of viral shedding in a study of 191 COVID-19 positive inpatients in China was 20 days; the longest duration observed was 37 days. Li Wenliang, MD, the whistleblower ophthalmologist who sounded the initial alarms on the coronavirus, and later died from the disease, believed he was infected by an asymptomatic glaucoma patient. The sum of these reports points to asymptomatic and presymptomatic transmission as a significant source of spread.
Environmental contamination by SARS-CoV-2 is another cause for concern. In a study published in the New England Journal of Medicine, scientists were able to detect viable SAR-CoV-2 in aerosols up to 3 hours post-aerosolization, although in an experimental setup lacking any ventilation, and not necessarily reflecting how the virus behaves in real-life conditions. The study also found infectious virus could survive up to 24 hours on cardboard, up to 4 hours on copper, and up to 2 to 3 days on plastic and stainless steel. In another study by the CDC of the recent cruise ship outbreaks of COVID-19, SARS-CoV-2 RNA (not necessarily indicating infectious virus) was identified on various surfaces within cabins of passengers who tested positive, for up to 17 days after they disembarked the ship.
In a report from the University of Nebraska, the authors used RT-PCR to test room air, personal articles and environmental surfaces for SARS-CoV-2 in the hospital rooms of COVID-19 patients. They found evidence of viral RNA throughout the rooms—even on windowsills and in ambient air. However, infectious virus could not be cultured from air samplers. These data emphasize the need to use personal protective equipment (PPE) meticulously, per local guidelines, and to remain vigilant in handwashing and disinfecting surfaces and materials possibly contaminated by respiratory secretions from infected patients.
Personal protective equipment (PPE) for ophthalmic use
There is heightened controversy regarding what constitutes appropriate PPE for ophthalmologists performing ophthalmic examinations, particularly around the use of masks and goggles. Reports of ophthalmologist and otolaryngologist deaths in China and Italy, new data about environmental virus contamination and increased awareness of asymptomatic and presymptomatic spread of new infections all favor mouth, nose, and eye protection. However, global shortages of PPE and concerns about mask effectiveness with extended wear and reuse have thus far impacted widespread adoption. Consequently, U.S. hospital guidance has varied from forbidding physicians from wearing masks except in high-risk interactions, presumably for fear of shortages, to mandating all hospital staff and patients wear surgical masks to reduce asymptomatic transmission. In hotspots, some hospitals require all caregivers to wear N-95 masks. The Academy relies on expert guidance from the CDC with regards to indications for extended mask wear and reuse. The use of masks during ophthalmic examinations is a rapidly evolving issue and our editors will update this page as new recommendations emerge.
Treatment and vaccine
Currently, there are no proven agents for prophylaxis or therapy for SARS-CoV-2 infection. Prominent among those under study are chloroquine and hydroxychloroquine, oral agents approved for malaria and autoimmune disorders, respectively, but concerns remain about potential cardiotoxicity. Remdesivir, an investigational antiviral drug, has shown promise in a recently published compassionate use study. Monoclonal antibody IL-6 receptor antagonists are being studied to address the “cytokine storm” seen in some patients with severe COVID-19. There are also efforts to use convalescent sera from COVID-19 survivors as therapy. More information about developments in the treatment of COVID-19 by these agents is available from the CDC.
At this time, there is no vaccine to prevent infection, but on March 5, mRNA coronavirus vaccine trials began enrollment at Kaiser Permanente Washington Health Research Institute in Seattle, and at Emory Children’s Center in Decatur. Both institutions are members of the Infectious Diseases Clinical Research Consortium, a clinical trials network supported by the National Institute of Allergy and Infectious Diseases (NIAID).
Use of chloroquine and hydroxychloroquine
The American Academy of Ophthalmology has no opinion on the use of chloroquine or hydroxychloroquine in COVID-19 patients. However, in a review of published guidelines for the use of these 2 drugs as treatment for COVID-19, a working group* from the Asia-Pacific Vitreo-Retina Society found that proposed doses in many of the ongoing studies worldwide exceeded the maximum daily dose considered safe for long-term therapy (generally <5mg/kg of real weight for hydroxychloroquine) for rheumatic and other chronic diseases (WF Mieler, MD, personal communication, March 25, 2020).
The risk of irreversible maculopathy at these higher doses for short periods of time is unknown. Patients should be informed of the potential for macular toxicity before starting therapy. Furthermore, the need for baseline fundus examination and/or imaging is also unknown in cases with high doses over a relatively short duration. Additional diagnostic testing, such as an ERG, prior to placing a patient on hydroxychloroquine for treatment of COVID-19 is likely unnecessary due to the short treatment duration. Additionally, performing an ERG in this setting carries an unnecessary risk of virus transmission. Until more is learned about the toxicity associated with current regimens, decisions should be made on an individual basis, taking into consideration any pre-existing retinal disease. As in all cases, the Academy urges ophthalmologists to make decisions guided by available scientific evidence.
* Ruamviboonsuk P, Lai T, Chang A, Lai C, Mieler W, Lam D
Updated Ophthalmology ties
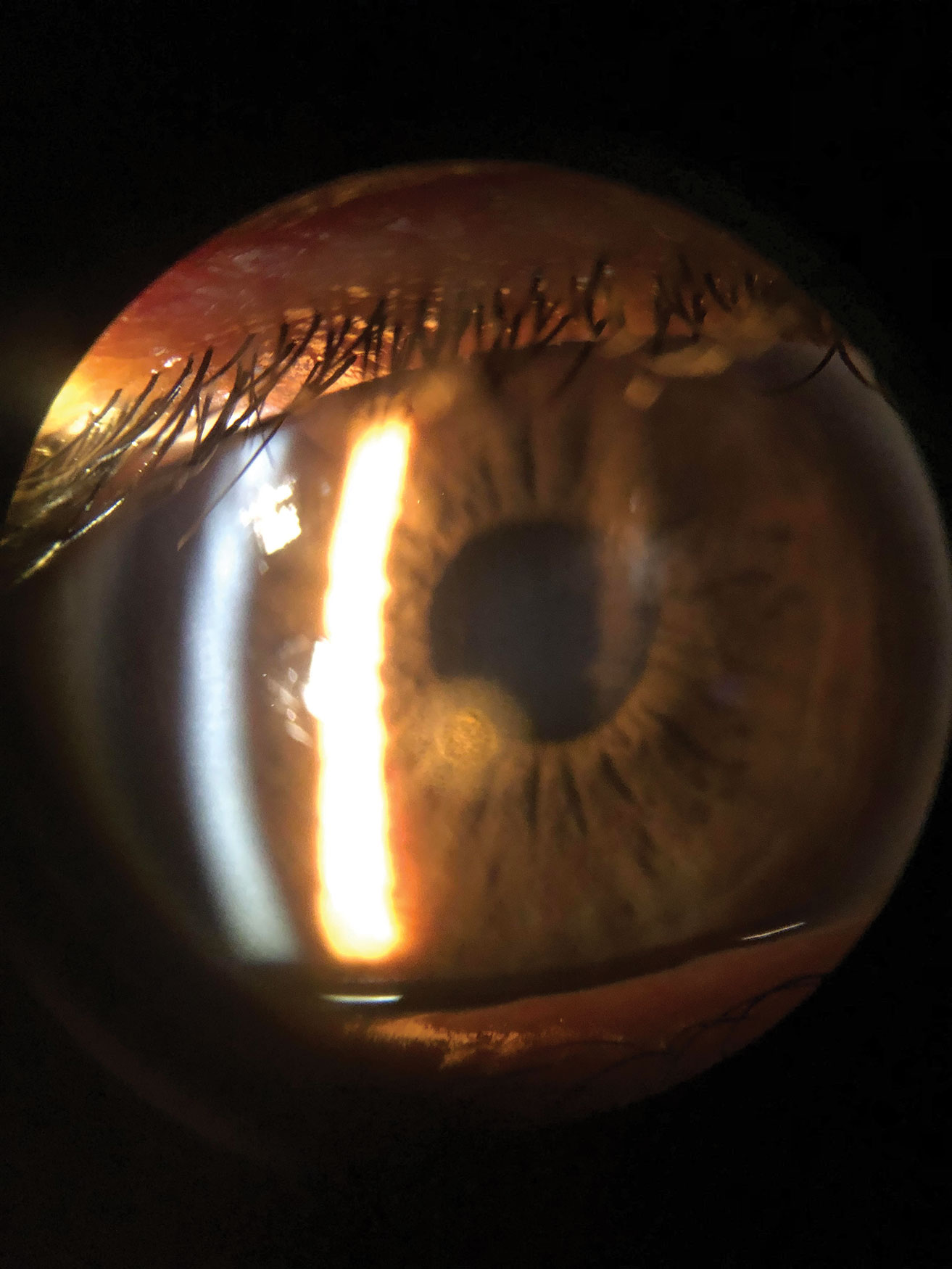
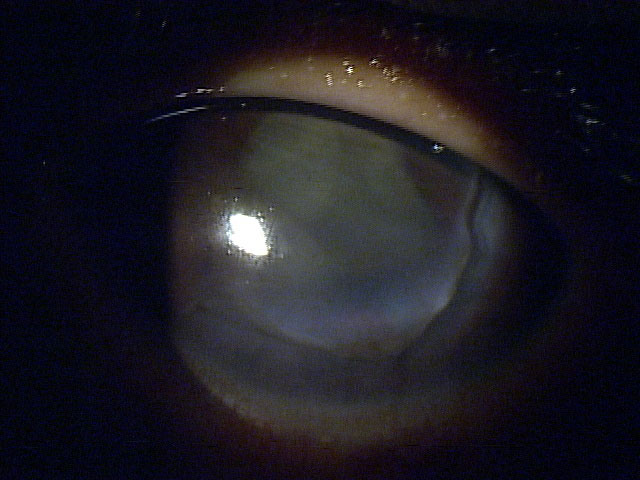
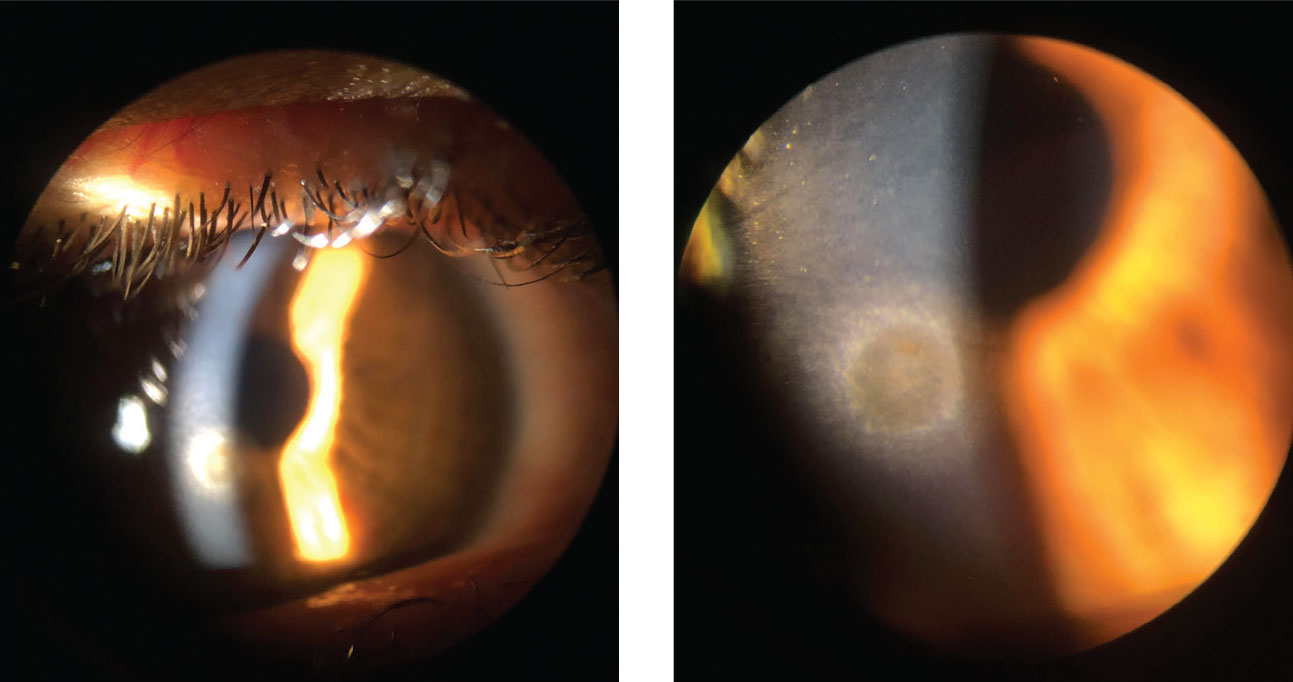
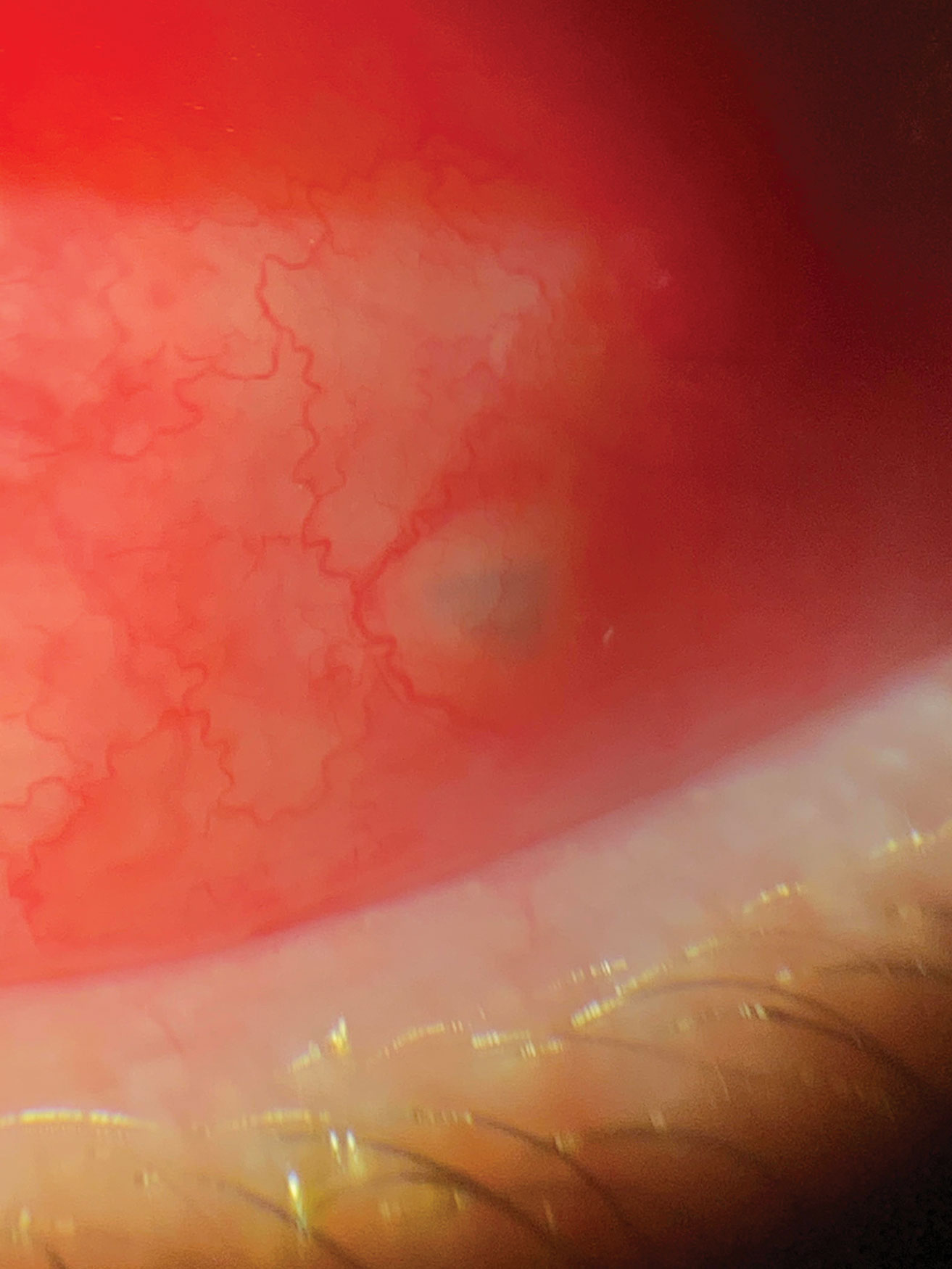
Several published reports and a recent news article suggest that SARS-CoV-2 can cause conjunctivitis, either as an early sign of infection, or during hospitalization for severe COVID-19 disease. Thus, it is possible that SARS-CoV-2 is transmitted to the conjunctiva by aerosol or through hand to eye contact. There is also evidence for SARS-CoV-2 RNA in tears of COVID-19 patients with conjunctivitis, although infectious virus has not yet been cultured from the conjunctiva of any COVID-19 patient.
- In a Journal of Medical Virology study of 30 patients hospitalized for COVID-19 in China, 1 had conjunctivitis. That patient—and not the other 29—had SARS-CoV-2 RNA in ocular secretions. This suggests that SARS-CoV-2 can cause conjunctivitis, and that infectious viral particles might be present in tears of COVID-19 patients with conjunctivitis. This observation was confirmed in a recent case report from China and another from Italy of patients with conjunctivitis in the setting of COVID-19.
- In a larger study published in the New England Journal of Medicine, researchers documented “conjunctival congestion” in 9 of 1,099 patients (0.8%) hospitalized with laboratory-confirmed COVID-19 from 30 hospitals across China. None of the patients were documented to have seen ophthalmologists, and tears were not sampled.
- In a retrospective case series published March 31 in JAMA Ophthalmology, 12 of 38 “clinically confirmed” hospitalized cases of COVID-19 in Hubei Province, China, had ocular “abnormalities,” characterized most commonly as chemosis and/or secretions. Two patients had a positive conjunctival swab for SARS-CoV-2 RNA, one with signs of conjunctival hyperemia and the other with chemosis and epiphora. This paper was discussed in the New England Journal of Medicine Journal Watch, which stated that “a third [of patients in the JAMA Ophthalmology paper] had conjunctivitis.” We disagree with the latter characterization; chemosis in a critically ill patient most likely represents third-spacing or fluid overload, not conjunctivitis.
- Two preprint studies posted on MedRxiv also suggest a relatively low likelihood of infectious virus in tears of COVID-19 patients. In a study by Zhang et al. of 72 confirmed COVID-19 patients at Tongji Medical College, 2 patients had conjunctivitis. One of the 2 with conjunctivitis and none of the other 70 patients had SARS-CoV-2 RNA in their tears. In a paper by Zhou et al. of 63 confirmed COVID-19 patients in Wuhan, only 1 had conjunctivitis; that patient had a negative conjunctival swab for SARS-CoV-2 RNA. One other patient’s conjunctival swab was positive and 2 were “probable.”
- In a case report published in the Annals of Internal Medicine, the first patient in Italy to be diagnosed with COVID-19 also had conjunctivitis in addition to fever and respiratory and gastrointestinal signs. RT-PCR on conjunctival swabs showed SARS-CoV-2 RNA from day 3 of hospitalization until day 21 (1 day after the conjunctivitis resolved), and again at day 27, at which point nasal swabs were negative. Infectious virus was isolated by cell culture from a sample taken on day 3.
- In a story from CNN, a registered nurse in a nursing home in Washington state with a large COVID-19 outbreak reported that red eye was a common early sign in elderly patients who then became sick with COVID-19.
Unless or until the CNN report is confirmed, existing data suggest that conjunctivitis is an uncommon event as it relates to COVID-19. However, because conjunctivitis is a common condition overall, and patients with conjunctivitis frequently present to eye clinics or emergency departments, it may happen that ophthalmologists are the first providers to evaluate patients possibly infected with COVID-19. Based on the studies above, it is possible that a patient with COVID-19 associated conjunctivitis could have infectious virus in their ocular secretions.
Therefore, protecting your mouth, nose (e.g., an N95 mask) and eyes (e.g., goggles or shield) is recommended when caring for patients potentially infected with COVID-19. In addition, slit-lamp breath shields (e.g., here ) are helpful for protecting both health care workers and patients from respiratory illness. Free slit-lamp breath shields are being offered by some manufacturers, including Topcon and Zeiss.
Questions you should ask to identify patients with possible exposure to SARS-CoV-2
- Does your patient have sore throat, fever, fatigue, loss of smell or respiratory symptoms?
- Has your patient been in the presence of someone with known COVID-19 in the last 2 to 14 days?
In regions currently managing significant outbreaks of COVID-19, it is safest to assume that any patient could be infected with SARS-CoV-2, and to proceed accordingly. The CDC is urging health care providers who encounter patients meeting these criteria to immediately notify both infection control personnel at your health care facility and your local or state health department.
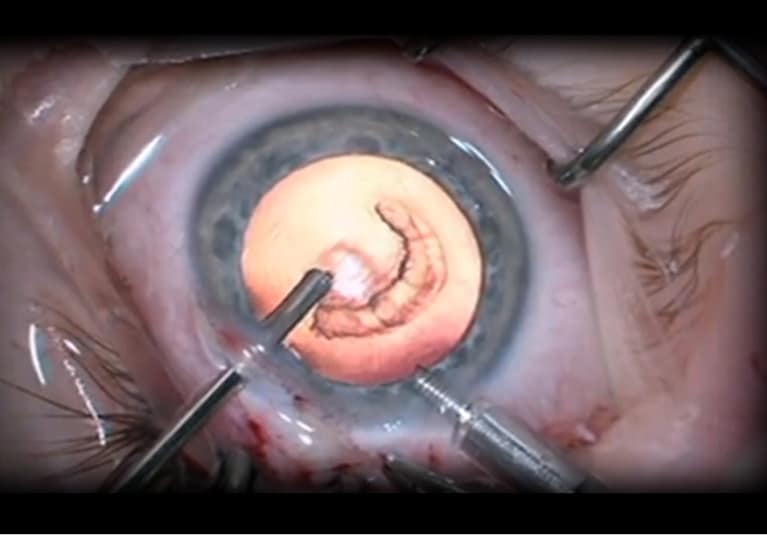
Outpatient clinics and elective surgery
On March 18, the Academy issued a statement urging all ophthalmologists to immediately cease providing any treatment other than urgent or emergent care. That statement was made based on recommendations from the American College of Surgeons and the CDC. Since then, based on the April 16 guidelines from the federal government, some facilities have begun to prepare for resuming elective surgeries.
Decisions on reopening eye clinics to routine care and resuming elective eye surgery will need to be made in consideration of numerous factors, as recently outlined by the American College of Surgeons and other leading medical organizations. These include but are not limited to evolving city and state restrictions to nonessential services, local/regional new case rates, availability of PPE and access to COVID-19 testing.
Read the full message from Academy CEO, David W. Parke II, MD, on reopening ophthalmology care.
Interim guidelines on resuming elective ophthalmic care
Until there is reliable point-of-care testing, an FDA-approved and highly effective therapy and/or an approved and effective vaccine, practices and clinics should continue to mandate social distancing in waiting rooms, frequent and meticulous disinfection of patient waiting and care areas, and the wearing of face coverings by both patients and caregivers. This means that clinic schedule volumes might need to remain below pre-COVID-19 levels for the foreseeable future. Additional precautions required in operating rooms may lead to longer turnover times between cases, thus impacting the number of surgical cases that can be performed per session. Presuming compliance with state and local regulations, the Academy recommends resumption of normal activities be undertaken gradually, in order to accommodate these and other as yet unforeseen issues.
The Academy also recognizes the potential role of serologic testing for ophthalmologists and other health care providers when considering resumption of elective visits and surgeries, but for now suggests caution in the interpretation of testing results. In response to the pandemic, current FDA policy allows developers to market serologic tests for antibodies to SARS-CoV-2. However, the FDA has not yet undertaken independent reviews of these tests for accuracy and reliability. A false-positive serologic test in an asymptomatic health care worker could leave them unknowingly at risk for COVID-19. Because humoral antibody responses to SARS-CoV-2 typically appear within 1 to 2 weeks of infection, while infected individuals can shed virus for up to 5 weeks from the onset of infection, a person with positive serology after asymptomatic infection might still be shedding virus and therefore remain infectious to patients and coworkers. It is also unknown to what degree a positive IgG response confers resistance to reinfection with SARS-CoV-2, and for how long. Finally, in regions with low prevalence of COVID-19, there is increased likelihood that a positive serologic test result would be an artifact or a testing error rather than reflect prior asymptomatic infection.
Recommended protocols when scheduling or seeing patients
- If the office setup permits, patients who come to an appointment should be asked prior to entering the waiting room about fever and respiratory illness and whether they or a family member have had contact with another person with confirmed COVID-19 in the past 2 to 14 days. If they answer yes to either question, they should be sent home and told to speak to their primary care physician about testing (see interim guidance below).
- Keep the waiting room as empty as possible, advise seated patients to remain at least 6 feet from one another. As much as prudent, reduce the visits of the most vulnerable patients.
- The use of commercially available slit-lamp barriers or breath shields is encouraged, as they may provide a measure of added protection against the virus. These barriers do not, however, prevent contamination of equipment and surfaces on the patient’s side of the barrier, which may then be touched by staff and other patients and lead to transmission. Homemade barriers may be more difficult to sterilize and could be a source of contamination.
- To further decrease the risk of viral spread, ophthalmologists should inform their patients that they will speak as little as possible during the slit-lamp examination, and request that the patient also refrain from talking.
- When examining patients, a surgical mask or cloth face covering for the patient, and a surgical mask and eye protection for the ophthalmologist are recommended.
- For any in-office procedures that require physical proximity to the patient (e.g., intravitreal injection, lateral tarsorrhaphy), regardless of the prevalence of COVID-19 in your area, the Academy recommends the patient wear a surgical mask or a cloth face covering if surgical masks are in short supply, and that the surgeon wear a surgical mask and eye protection. An N95 mask for the surgeon can be considered if not in short supply. The CDC’s recommendations on N95 extended use and/or reuse should be followed.
- Because U.S. testing for SARS-CoV-2 infection remains sporadic and for the most part has been made available only to those with stereotypical symptoms, the true regional prevalences of SARS-CoV-2 within the United States remain mostly unknown. Therefore, for surgical procedures that may generate aerosolized virus, preoperative testing (RT-PCR) for asymptomatic patients, and the use of N95 masks (and eye protection) by operating room personnel should be considered. For cases that require general anesthesia, personnel not in N95 masks should remain out of the OR during intubation/extubation. For non-aerosolizing procedures performed under monitored anesthesia/conscious sedation, the patient should be placed in a surgical mask. Because of prolonged proximity of the eye surgeon to the patient, the surgeon can consider wearing an N95 mask if supplies permit.
- Increasingly, ophthalmologists will be asked to examine and perform office-based procedures on patients who have recovered or are recovering from COVID-19. Because viral shedding can be prolonged (up to 37 days in one study), repeat testing (RT-PCR performed on a nasopharyngeal swab) is recommended for patients prior to treatment if less than 6 weeks from COVID-19 diagnosis, except in emergent circumstances. If the repeat SARS-CoV-2 test is positive, delayed or not available, the patient should wear a surgical mask. The treating ophthalmologist should wear an N95 mask, rather than a surgical mask, in addition to gown, gloves and eye protection.
- The CMS and HHS have allowed for the expanded use of telehealth services during the COVID-19 public health crisis. For more information on telephone services, internet-based consultation or telemedicine exam, visit the Academy’s Coding for Phone Calls, Internet and Telehealth Consultations.
Interim guidance for triage of ophthalmology patients
Clinical Situation
|
Patient Management / Precautions
|
| 1. Routine ophthalmic issues and previously scheduled appointments |
- Appointments should be rescheduled only upon clearance from public health authorities.
- Refill all necessary medications.
|
| 2. Urgent ophthalmology appointment for a patient with no respiratory illness symptoms, no fever, and no COVID-19 risk factors |
- Standard precautions.*
- Added precaution of not speaking during slit-lamp biomicroscopic examinations is appropriate.
- In the setting of adequate PPE supplies, use of surgical mask and eye protection** for the clinician as well as surgical mask for the patient may reduce asymptomatic and presymptomatic transmission.
|
| 3. Urgent ophthalmic problem in a patient with respiratory illness symptoms, but no fever or other COVID-19 risk factor |
- The patient can be seen in the eye clinic.
- The patient should be placed in an examination lane immediately with the door closed and placed in a surgical mask. The treating ophthalmologist and health care personnel require surgical masks at minimum.
- Gown, gloves, surgical mask and eye protection are recommended for the clinician.† An N95 mask should be worn if a procedure is planned that will result in aerosolized virus.
- The examining room must be disinfected after examination.
|
| 4. Urgent ophthalmic problem in a patient who is at high risk for COVID-19 |
- The patient is best sent to the ER or other hospital-based facility equipped to evaluate for, and manage, COVID-19.
- If the patient has an urgent eye problem based on screening questions, the facility should be one that is equipped to provide eye care in the hospital setting.
- If SARS-CoV-2 infection is confirmed, CDC (or hospital) guidelines for care of suspected COVID-19 patients should be followed for health care facility preparation and infection control.
- Eye care is best provided in the hospital setting. Transmission precautions‡ for treating ophthalmologists include wearing a surgical mask, gown, gloves and eye protection (face shield or goggles, if available).
|
| 5. Urgent ophthalmic problem in a patient with documented COVID-19 (or person under investigation [PUI]) |
- The patient should remain in the hospital setting if possible.
- Determine whether the eye problem is urgent based on screening questions, and if so, evaluation and management should be in the hospital setting.
- If the patient is not hospitalized at the time of referral, the patient is best referred to the ER or other hospital-based facility equipped to manage both COVID-19 and eye care.
- CDC or hospital guidelines should be followed for care of COVID-19 patients.
- Transmission precautions† for treating ophthalmologists include wearing an N95 mask, gown, gloves and eye protection (face shield or goggles, as above).
[Read the American College of Surgeon’s guidelines for operating on COVID-19 patients] |
* Standard (Universal) Precautions: Minimum infection prevention precautions that apply to all patient care, regardless of suspected or confirmed infection status of patient, in any health care setting (e.g., hand hygiene, cough etiquette, use of PPE, cleaning and disinfecting environmental surfaces). See CDC: Standard Precautions.
** Supply permitting, tight-fitting goggles may be preferable to face shields for eye protection.
† Currently, there are worldwide shortages of personal protective equipment (PPE), which also warrant consideration. Excessive use of PPE may deplete the supply of critical equipment required for patients with COVID-19 as the epidemic expands. Use of PPE should be considered on an institutional and case-by-case basis; universal usage for all patient encounters is appropriate in regions with particularly high COVID-19 prevalence. Surgical masks reduce asymptomatic transmission by the person wearing the mask. N95 masks reduce infection of the person wearing the mask. Note that although the FDA now permits importation of Chinese-made N95 masks as an alternative to those made in the United States, recent reports caution that some masks may not meet U.S. quality standards.
‡ Transmission Precautions: Second tier of basic infection control, used in addition to Standard Precautions when patients have diseases that can spread through contact, droplet or airborne routes, requiring specific precautions based on the circumstances of a case. Transmission precautions are required for cases of suspected COVID-19. See CDC: Transmission-Based Precautions.
Environmental cleaning and disinfection recommendations
Rooms and instruments should be thoroughly disinfected after each patient encounter. Manufacturers’ guidance should be followed when cleaning delicate diagnostic equipment such as visual field analyzers. Wear disposable gloves when cleaning and disinfecting surfaces, and discard the gloves after use. Slit lamps, including controls and accompanying breath shields, should be disinfected, particularly wherever patients put their hands and face. The current CDC recommendations for disinfectants specific to COVID-19 include:
- Diluted household bleach (5 tablespoons bleach per gallon of water)
- Alcohol solutions with at least 70% alcohol.
- Common EPA-registered household disinfectants currently recommended for use against SARS-CoV-2 include Clorox brand products (e.g., disinfecting wipes, multi-surface cleaner + bleach, clean up cleaner + bleach), Lysol brand products (e.g., professional disinfectant spray, clean and fresh multi-surface cleaner, disinfectant max cover mist), Purell professional surface disinfectant wipes and more. The EPA offers a full list of antimicrobial products expected to be effective against COVID-19 based on data for similar viruses.
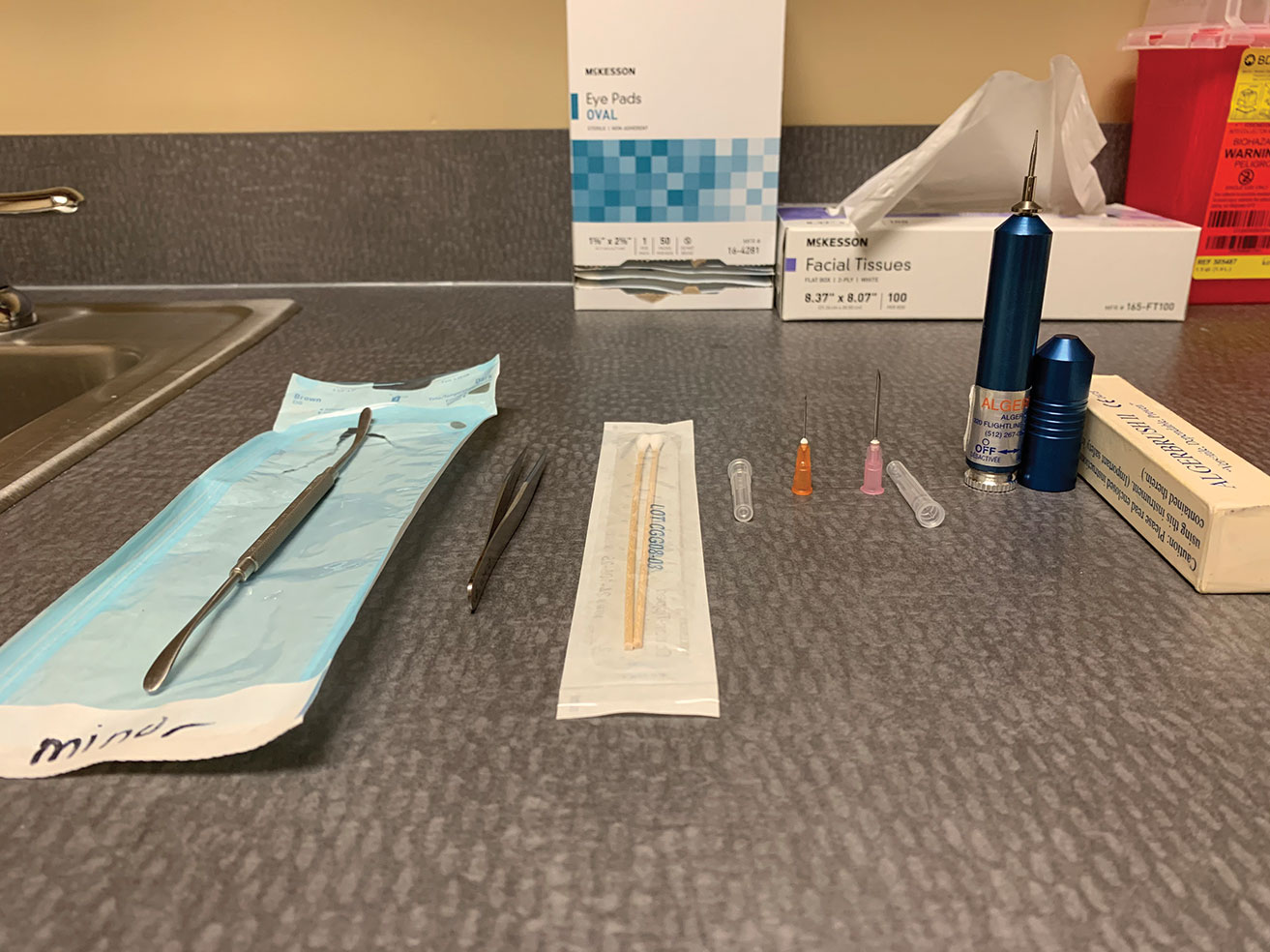
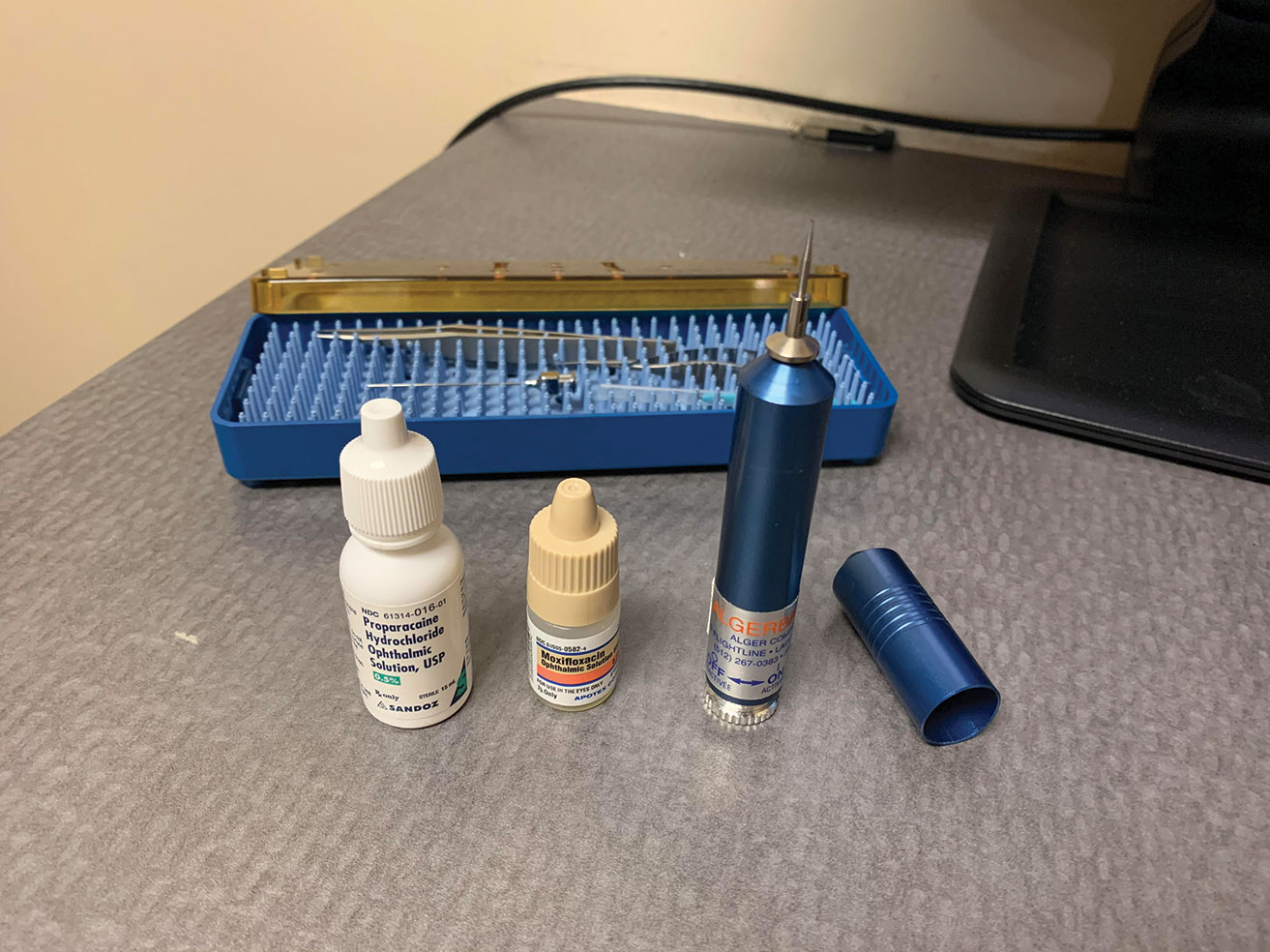
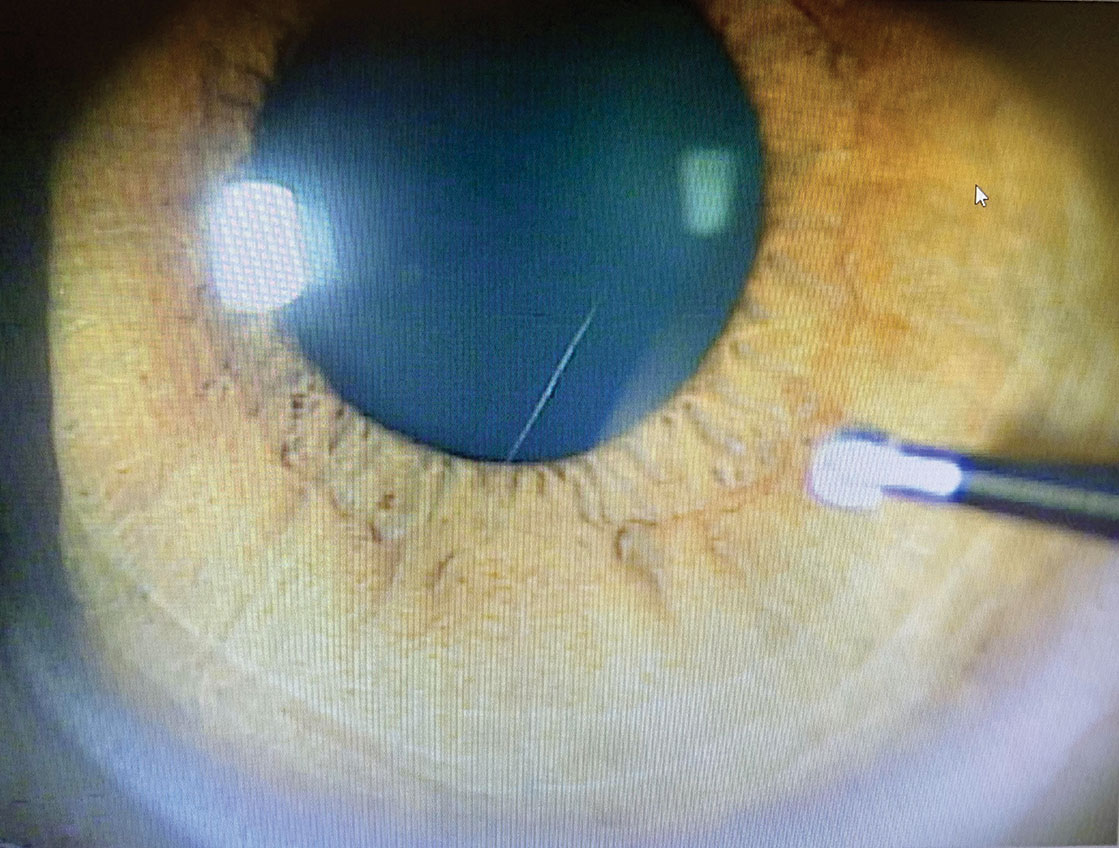
Tonometer tip cleaning
The virus causing COVID-19 is an enveloped virus, unlike adenoviruses that are much more resistant to alcohol. If a tonometer tip is cleaned with alcohol and allowed to dry in room air, 70% alcohol solutions should be effective at disinfecting tonometer tips from SARS-CoV-2. However, alcohol will not effectively sterilize the tip against adenoviruses. Use single-use, disposable tonometer tips if available. Tips cleaned with diluted bleach remain a safe and acceptable practice.
Multidose eye drops
For diagnostic eye drops required for ophthalmic examinations, multidose eye drop containers should be kept in cabinets or other closed spaces away from anywhere that could become contaminated during a patient encounter. As should always be the case, care must be taken not to touch the eyelashes or ocular surface with the tip of the eye drop bottle, and the examiner’s hands should be disinfected immediately after touching the patient’s face.
Resources
WHO
CDC
For ophthalmologists filling critical care roles
Ophthalmic subspecialty-specific recommendations
Relevant articles
EyeNet magazine
- Of Black Swans, TP, and Health Care, editorial by David W. Parke II, MD, CEO
- COVID-19 and Ophthalmology, editorial by David W. Parke II, MD, CEO
- Reflections During a Crisis, editorial by Ruth D. Williams, MD, Chief Medical Editor
- COVID-19 Moves Telemedicine to the Forefront
- COVID-19 Pandemic: Ocular Tumor Triage and Care
Journal studies and scientific articles
If you have practical, clinical experience to share about the COVID-19 outbreak, email onefeedback@aao.org. The site editors will review and post items that will benefit the community.
James Chodosh, MD, MPH, is the David G. Cogan Professor of Ophthalmology at Harvard Medical School’s Department of Ophthalmology, a member of Harvard’s PhD program in virology and an expert in cornea and external disease.
Gary N. Holland, MD, is the Jack H. Skirball Professor of Ocular Inflammatory Diseases, director of the Ocular Inflammatory Disease Center, and a member of the cornea/external disease and uveitis divisions at the Jules Stein Eye Institute, David Geffen School of Medicine at UCLA.
Steven Yeh, MD, is the M. Louise Simpson Associate Professor of Ophthalmology, a member of the uveitis and vitreoretinal surgery divisions at the Emory Eye Center, and a faculty fellow of the Emory Global Health Institute.
Photo Credit: Content Providers(s): National Institute of Allergy and Infectious Diseases (NIAID) – This media comes from the Centers for Disease Control and Prevention‘s Public Health Image Library (PHIL), with identification number #18109.